ABSTRACTS
Does Weight Bias Impact the Quality of EMS Treatment? Good News and Bad NewsAuthor: Jamie Kennel, PhD, MAS, Paramedic | | Associate Authors:
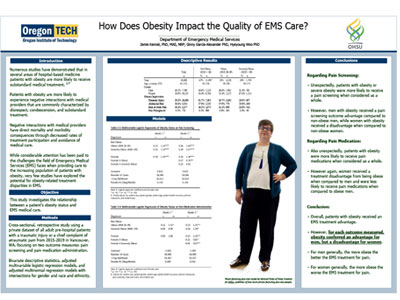
Introduction While considerable attention has been paid to the challenges Emergency Medical Services (EMS) faces when providing treatment to patients with obesity, very few studies have explored the potential for treatment disparities. Studies have demonstrated that in several areas of medicine weight bias is associated with substandard medical treatment; however, there is a paucity of research regarding weight bias in EMS. This study investigates the relationship between a patient’s obesity status and the quality of their EMS medical treatment. Methods We conducted a cross-sectional, retrospective study using a private dataset of adult prehospital patients with a traumatic injury or a chief complaint of atraumatic pain from 2015-2019 in Vancouver, WA, focusing on three outcome measures: pain screening, pain medication administration, and pain reduction. The data were analyzed using bivariate descriptive statistics, adjusted multivariable logistic regression models, and adjusted multinomial regression models with intersections for gender and race/ethnicity. During the timeframe studied, 11,987 patients without obesity and 6013 patients with obesity were examined by EMS clinicians. In multivariable models adjusted for demographic and clinical characteristics, patients with obesity (aOR 1.24, P < .001) or severe obesity (aOR 1.29, P < .001) were more likely to receive a pain screening. Further, patients with obesity were more likely to receive pain medications (aOR 1.11, P <.01) and patients with severe obesity were more likely to be in increased pain (aOR 1.38, P < .01) at the conclusion of their EMS encounter. However, the obesity “advantage” in EMS treatments is considerably stronger for men with obesity, while women with obesity see a minor advantage in pain screening but an obesity “disadvantage” in relation to pain medication administration and pain reduction at the conclusion of their EMS encounter when compared to men. Results Surprisingly, our results indicate that obesity status may provide a treatment advantage to male patients, while female patients may not receive this advantage across treatment measures. We suspect that bias against obese patients may play a role in treatment disparity for female patients in EMS as has been found in other domains of medical care. Limitations, implications, and future research directions are discussed.
|