ABSTRACTS
Improved Decision Making in Transport of Hypoxemic Patients Using CQI ProcessesAuthor: Todd Costa | | Associate Authors: Linda Verraster | Brandon Grinstead | Claus Hecht
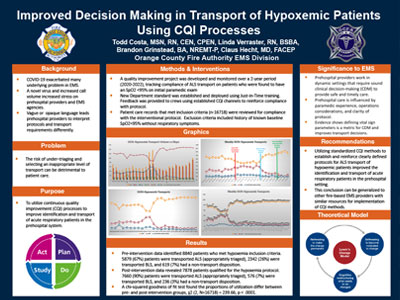
Introduction Prehospital providers work in dynamic settings that require sound clinical decision-making (CDM) to provide safe and timely care. Prehospital care is influenced by paramedic experience, operations considerations, and clarity of protocol. The risk of under-triaging and selecting an inappropriate level of transport can be detrimental to patient care. Evidence shows defining vital sign parameters is a metric for CDM and improves transport decisions. Pulse oximetry (SpO2) is one vital sign that is an accurate indicator of acuity in respiratory patients. Using Continuous Quality Improvement (CQI) methods, a fire-based emergency medical services (EMS) team that oversees care of 110,000 EMS calls per year disseminated defined pulse oximetry guidelines as a method to improve identification and transport of acute respiratory patients in the prehospital system. Methods A quality improvement project was developed and monitored over a 2-year period (2020-2022), tracking compliance of advanced life support (ALS) transport on patients who were found to have an SpO2 < 95% on initial paramedic exam. Patient care records that met inclusion criteria (N = 16,718) were reviewed for compliance with the interventional protocol. Exclusion criteria included history of known baseline SpO2 < 95% without respiratory symptoms. Feedback was provided to crews using established CQI channels to reinforce compliance with protocol. A chi-squared goodness of fit test was conducted to analyze the pre- and postimplementation groups. Results Preintervention data identified 8840 patients who met hypoxemia inclusion criteria, of whom 5879 (67%) patients were transported ALS (appropriately triaged), 2342 (26%) were transported BLS, and 619 (7%) had a nontransport disposition. Postintervention data revealed 7878 patients qualified for the hypoxemia protocol; 7660 (90%) patients were transported ALS (appropriately triaged), 576 (7%) were transported BLS, and 236 (3%) had a nontransport disposition. A chi-squared goodness of fit test found the proportions of utilization differ between preintervention and postintervention groups, (P < .0001). Conclusion Utilizing standardized CQI methods to establish and reinforce clearly defined protocols for ALS transport of hypoxemic patients improved the identification and transport of acute respiratory patients in the prehospital setting. This conclusion can be generalized to other fire-based EMS providers with similar resources for implementation of CQI methods.
|