ABSTRACTS
Do Trauma Patients Receive Better EMS Treatment If They Speak English? It Shouldn’t Matter, But It DoesAuthor: Jamie Kennel | | Associate Authors: Adam Wagner
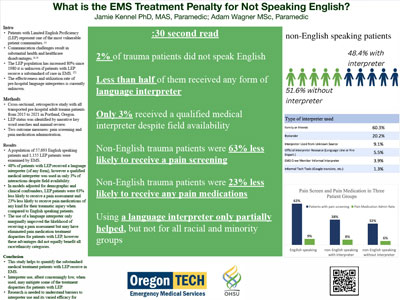
Introduction Traumatic injury causes significant acute and chronic pain, and accurate pain assessment and treatment is critical for quality patient management. Prior studies have revealed disparities in the treatment of pain by race and ethnicity in Emergency Medical Services (EMS), but the effect of patient language on pain management remains unknown. This study investigates the relationship between Limited English Proficiency (LEP) and pain treatment for prehospital trauma patients and examines the effects language interpretation may have on pain treatment. Methods We conducted a cross-sectional, retrospective study using a private dataset that included all prehospital adult trauma patients from 2015 to 2021 at a single urban/suburban EMS agency in Portland, Oregon. Patient language, numeric pain scores, pain medication utilization, interpreter status, demographic, and clinical covariates were extracted from the EMS patient care record. We used adjusted multivariable logistic regressions to compare pain assessment and pain medication administration between LEP and English proficient patients while also exploring race and gender variations. Results During the timeframe studied 57,693 English speaking patients and 1155 LEP patients were examined by EMS clinicians. In multivariable models adjusted for demographic and clinical characteristics, LEP patients were less likely to receive a pain assessment (aOR 0.37, P < .001), and less likely to receive any pain medications (aOR 0.77, P < .01) when compared to English-speaking patients. Further, patients with LEP received a qualified medical interpreter only 3% of the time and any form of interpreter 48% of the time. Finally, the use of a language interpreter marginally improved the likelihood of receiving a pain assessment but may have eliminated pain medication treatment disparities for patients with LEP; however, these advantages did not equally benefit all race/ethnicity categories. Conclusion Patients with LEP represent some of the most vulnerable patients as they experience numerous marginalized intersecting identities in addition to a communication barrier. For the first time, this study quantifies the substandard medical treatment patients with LEP receive in EMS. This study also finds encouraging evidence that use of a language interpreter may mitigate some of the treatment impacts for some but not all racial/ethnic minority patients. Limitations, implications, and future research directions are discussed.
|