ABSTRACTS
Whole Blood versus Blood Components in Prehospital CareAuthor: Scott Kostolni | | Associate Authors: Linh T. Nguyen MD, Tamara Klindt MPH NREMTP, Iv Godzdanker MD, David Wampler PhD LP FAEMS, Sharon Long MD Lawrence Brown PhD
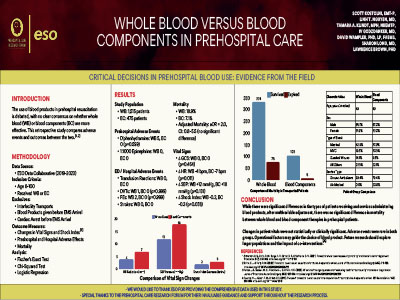
Background: There is no consensus on whether resuscitation with whole blood (WB) or blood components (BC) (Packed Red Blood Cells (PRBCs), Fresh Frozen Plasma (FFP), or Platelets) is the safest and most effective for prehospital patients. This study aimed to compare the frequency of adverse events and outcomes for prehospital patients receiving WB or BC. Results: There were 1,515 eligible patients who received WB and 475 who received one or more BC (PRBC & FFP = 103; PRBCs only = 313; FFP only = 20; unspecified = 39). Five WB patients and no BC patients received diphenhydramine (0.3% vs. 0.0%, p=0.599); no patients received epinephrine. ED/hospital diagnosis data were available for 381 WB and 129 BC patients. There were no reports of transfusion reactions. One WB patient had a DVT (0.3% vs. 0.0%, p=0.999), and two WB patients had a PE (0.5% vs. 0.0%, p=0.999). There were no reported strokes. Observed mortality was higher in the WB group (19% vs 7%), but after adjustment, the difference was not statistically significant (aOR = 2.0, CI: 0.8–5.5). The limitations of this study include a retrospective study design and small sample size. Conclusion: Adverse events are equally rare following prehospital administration of WB or BC, and differences in mortality appear attributable to patient and encounter characteristics. These findings suggest EMS agencies seeking to use whole blood or blood products may consider either option, depending on logistical or operational constraints.
|