ABSTRACTS
Intraosseous Route Prolongs Epinephrine-to-ROSC Interval in Out-of-Hospital Cardiac ArrestAuthor: Jewel Williams, Matthew Crittenden, Diana-Truc Nguyen, Stephen Taylor, Michael W. Hubble | | Associate Authors:
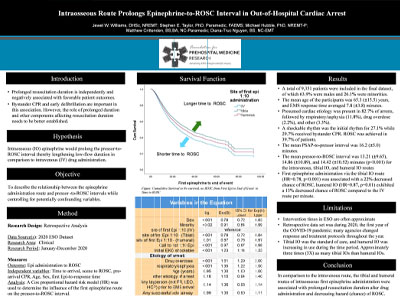
Introduction: Prolonged duration of resuscitation is independently associated with less favorable patient outcomes. While the importance of bystander CPR and early defibrillation are well-known, the role of other components potentially affecting resuscitation duration is less well established. We hypothesized that intraosseous (IO) epinephrine would prolong the pressor-to-return of spontaneous circulation (ROSC) interval, lengthening the low-flow duration compared to intravenous (IV) drug administration. Objective: To describe the relationship between the epinephrine administration route and pressor-to-ROSC intervals while controlling for potentially confounding variables. Methods: A retrospective analysis was conducted using the 2020 ESO dataset containing all calls from January through December 2020. The sample included adults who experienced nontraumatic, bystander-witnessed arrests prior to EMS arrival and who received one or more boluses of epinephrine via either IO or IV routes. A Cox proportional hazard model was used to determine the association between the first epinephrine route and the pressor-to-ROSC interval while controlling for potentially confounding variables. End-of-event was defined as ROSC, field termination of resuscitation, or hospital arrival without ROSC, with right censoring of the latter group. Results: Overall, 9351 patients were included in the final dataset, of which 63.9% were males and 26.1% were minorities. The mean age of the participants was 65.3 (± 15.5) years, and EMS response time averaged 7.8 (± 3.8) minutes. Presumed cardiac etiology was present in 82.7% of arrests, followed by respiratory/asphyxia (11.8%), drug overdose (2.2%), and other (3.3%). A shockable rhythm was the initial rhythm for 27.1%, while 29.7% received bystander CPR. ROSC was achieved in 39.7% of patients. The mean PSAP-to-pressor interval was 16.2 (± 5.0) minutes. The mean pressor-to-ROSC interval was 13.21 (± 9.65), 14.86 (± 10.89), and 14.42 (± 10.52) minutes (p < .001) for the intravenous, tibial IO, and humeral IO routes, respectively. After controlling for potential confounders, first epinephrine administration via the tibial and humeral IO routes were associated with decreased hazard of ROSC compared to the IV route (HR = 0.78, p < .001 and HR = 0.86, p = .01 per minute, respectively). Conclusion: Our data suggest that, in comparison to the intravenous route, the tibial and humeral routes of intraosseous first epinephrine administration were associated with longer resuscitation duration after drug administration and decreasing hazard of ROSC.
|