ABSTRACTS
A Comparison of the Accuracy of Different Resuscitation Termination Criteria for Out-of-Hospital Cardiac Arrest Patients in Bangkok, ThailandAuthor: Phatcha Termkijwanich, Pungkawa Sricharoen, Pitsucha Sanguanwit, and Chaiyaporn Yuksen | | Associate Authors:
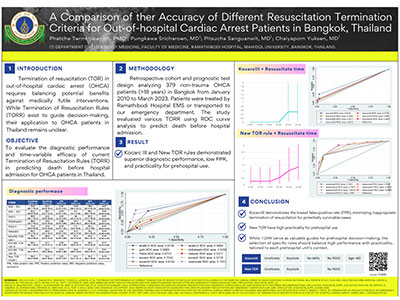
Introduction: Termination of resuscitation (TOR) in out-of-hospital cardiac arrest (OHCA) requires balancing potential benefits against medically futile interventions. Although termination of resuscitation rules (TORR) exist to guide decision-making, their application to OHCA patients in Thailand remains unclear. Objective: To investigate the effectiveness of current TORR, which incorporate factors assessable in the prehospital setting, for OHCA patients in Thailand. Methods: This diagnostic, retrospective cohort study analyzed 379 out of 414 nontrauma OHCA patients (> 18 years) in Bangkok. Patients were either treated by the EMS of Ramathibodi Hospital, a university-based tertiary care center (January 2021–March 2023) or transported to Ramathibodi's emergency department by other EMS providers (January 2010–March 2023). Patients with obvious signs of death or do-not-resuscitate orders were excluded. The study evaluated the discrimination and diagnostic indices of various TORR in predicting death before hospital admission using ROC curve analysis. Results: Among 379 OHCA patients, 308 (81.27%) died before hospital admission. Of 10 TORR evaluated, the New TOR model showed the best performance (AUC = 0.74, 95% CI = 0.70–0.79), with high sensitivity (96.7%, 95% CI = 93.0–98.8) and negative predictive value (NPV) (91.5%, 95% CI = 82.5–96.8), and, respectively, specificity 33.2% (95% CI = 26.6–40.2) and positive predictive value (PPV) (57.5% (95% CI = 51.5–63.1). The AHA–BLS criteria ranked second (AUC = 0.67, 95% CI = 0.62–0.73), with lower sensitivity (92.0%, 95% CI = 87.1–95.4) and NPV (78.9%, 95% CI = 67.6–87.7), and, respectively, specificity 29.2% (95% CI = 22.8–36.1) and PPV 55.8% (95% CI: 50.1–61.5). Conclusion: The New TOR model demonstrated the best performance among 10 TORR evaluated in predicting death before hospital admission for OHCA patients. Its high sensitivity and negative predictive value suggest potential utility in guiding prehospital decisions. However, it should be used in conjunction with clinical judgment to prevent erroneous TOR. As these criteria lack specific evaluation time points, future studies should assess long-term outcomes and its applicability at various time points to validate its effectiveness in Thai EMS systems.
|