ABSTRACTS
Evaluating Prehospital Care for Patients with Asthma-Related EMS Impressions in Washington, DCAuthor: Maura Nakahata, Daniel P. Burke, Alison Treichel, Jennifer K. Wilson, Christopher Montera, J. Brent Myers, and Antonio R. Fernandez | | Associate Authors:
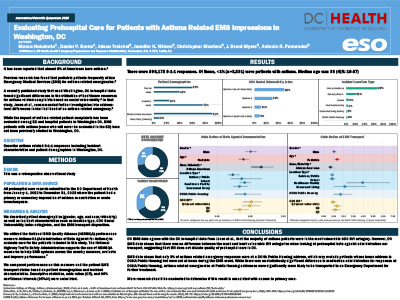
Introduction: Washington, DC (DC) emergency department (ED) and hospital patients with asthma have been previously evaluated, but DC emergency medical service (EMS) patients with asthma have not. Objective: To describe patient care and transport for asthma-related 9-1-1 responses in DC. Methods: This retrospective study included all 9-1-1 responses in DC from January 1, 2022, to December 31, 2023, with an EMS impression of asthma exacerbation or acute bronchospasm. Outcomes of interest included beta agonist administration and EMS transport. We utilized the National EMS Quality Alliance performance measure (Asthma-01) to evaluate beta agonist administration. We compared performance based on patient demographics and incident characteristics. Descriptive statistics, odds ratios (ORs), and 95% confidence intervals (95% CIs) were calculated. Results: A total of 3531 responses for asthma were evaluated. Most patients were female (60%). Median age was 33 years (IQR = 18–57). Twenty-four percent were pediatric patients; 91% had race/ethnicity documented as Black/African American; and 3% were in public housing. Fifty percent were in the most vulnerable CDC Social Vulnerability Index (CDC-SVI) category, while 9% were in the least vulnerable category. Overall, 72% received a beta agonist. There was a 21% decrease in odds of administration for pediatrics compared to adults (OR = 0.79, 95% CI = 0.66–0.94). Odds increased 33% when race/ethnicity was documented as Black/African American compared to all other race/ethnicities (OR = 1.33, 95% CI = 1.05–1.69). Odds of administration were similar when comparing public housing status (OR = 0.84, 95% CI = 0.54–1.32) and when comparing CDC-SVI categories (OR = 1.03, 95% CI = 0.79–1.34). Thirty-three percent were not transported by EMS; of those, 73% refused transport. Pediatric odds of transport were increased by 35% compared to adults (OR = 1.35, 95% CI = 1.14–1.60). The odds of transport were decreased 32% among those whose race/ethnicity was Black/African American when compared to all other race/ethnicities (OR = 0.68, 95% CI = 0.53–0.88). There was a 69% increase in the odds of transport when comparing those in public housing to those who were not in public housing (OR = 1.69, 95% CI = 1.03–2.76). Odds of transport were similar when comparing CDC-SVI categories (OR = 0.93, 95% CI = 0.72–1.19). Conclusion: DC EMS data agrees with the DC in-hospital findings that the majority of asthma patients were in the most vulnerable CDC-SVI category. However, DC EMS data did not reflect differences between the most and least vulnerable SVI categories for prehospital beta agonist administration or transport.
|