ABSTRACTS
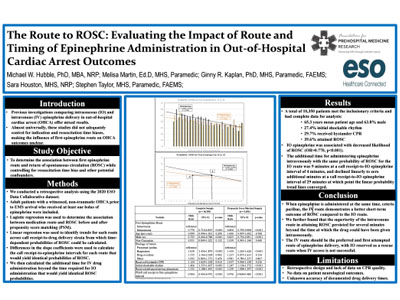
The Route to ROSC: Evaluating the Impact of Route and Timing of Epinephrine Administration in Out-of-Hospital Cardiac Arrest OutcomesAuthor: Michael W. Hubble, Melisa D. Martin, Ginny R. Kaplan, Sara E. Houston, and Stephen Taylor | | Associate Authors:
Introduction: Previous investigations comparing intraosseous (IO) and intravenous (IV) epinephrine delivery in out-of-hospital cardiac arrest (OHCA) have offered mixed results. Almost universally, these studies did not adequately control for indication and resuscitation time biases, clouding the association between first epinephrine route on OHCA outcomes. Objective: To explore the association between first epinephrine route and return of spontaneous circulation (ROSC) while controlling for resuscitation time bias and other potential confounders. Methods: A retrospective analysis was conducted using the 2020 ESO Data Collaborative dataset. Adult patients with a witnessed, nontraumatic OHCA prior to emergency medical services (EMS) arrival who received at least one bolus of epinephrine were included. Logistic regression was used to determine the association between medication route and ROSC before and after propensity score matching (PSM). Linear regression was used to identify trends for each route across call receipt-to-drug delivery strata from which time-dependent probabilities of ROSC could be calculated. Results: Data were available for 10,350 patients: 63.8% were male, 27.4% presented with a shockable rhythm, and 83.8% had a cardiac etiology. The mean age of participants was 65.3 (± 15.6) years. Altogether, bystander CPR was performed in 29.7% of cases, and 39.6% experienced ROSC. After controlling for call receipt-to-first epinephrine interval and other confounders, epinephrine administered via the IO route was associated with decreased likelihood of ROSC (OR = 0.770, p < .001). Similar results were obtained after PSM. Linear regression models indicated differing slope coefficients for ROSC between the IV and IO routes from which the additional time allowed to establish an IV and administer epinephrine intravenously for an equivalent predicted probability of ROSC via IO route could be calculated. This additional time interval declined linearly from 9 minutes at a call receipt-to-IO epinephrine interval of 4 minutes to essentially no additional time at a call receipt-to-IO epinephrine interval of 29 minutes, at which point the trend lines converged. Conclusion: This retrospective analysis of a national EMS database revealed that IO epinephrine administration was negatively associated with ROSC. Additionally, there appears to be a finite time window during which IV epinephrine remains superior to the IO route even if there are brief initial delays in IV drug delivery.
|