ABSTRACTS
Examining Pediatric EMS Care in North Dakota Using National EMS Quality Alliance MeasuresAuthor: Chettie Greer, Christopher T. E. Price, Alison Treichel, Remle P. Crowe, J. Brent Myers, Jennifer K. Wilson, Christopher Montera, and Antonio R. Fernandez | | Associate Authors:
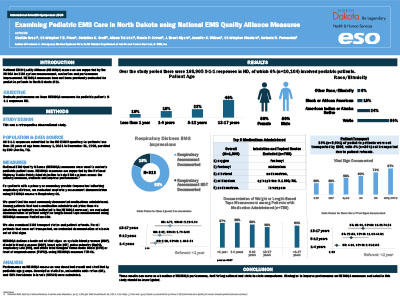
Introduction: National EMS Quality Alliance (NEMSQA) measures are supported by the National Highway Traffic Safety Administration (NHTSA) for EMS system measurement, evaluation, and performance improvement. NEMSQA measures have not been previously evaluated for pediatric patients in North Dakota. Objective: To evaluate performance on three NEMSQA measures for pediatric patient 9-1-1 responses in North Dakota. Methods: This retrospective analysis evaluated all 9-1-1 responses submitted to the North Dakota EMS Repository for patients younger than 18 years from January 1, 2021, to December 31, 2023. Respiratory assessment documentation (Respiratory-01) was evaluated for patients with a provider impression indicating respiratory distress. Documentation of patient weight/length-based tape measurement among those who received medication by EMS (excluding inhalation or topical, as per NEMSQA measure: Pediatrics-03b) was evaluated. Among nontransported patients, vital signs were evaluated, per TTR-01 (documentation of basic set of vital signs [BSVS]: systolic blood pressure [SBP], diastolic blood pressure [DBP], heart rate [HR], pulse oximetry [SpO2], respiratory rate [RR], and either total Glasgow Coma Scale Score [GCS] or level of responsiveness [AVPU]). Descriptive statistics, univariate odds ratios (OR), and 95% confidence intervals (95% CI) were calculated. Results: A total of 168,905 9-1-1 responses were evaluated, of which 6% (n = 10,104) involved pediatric patients: 10% < 1 year, 18% 1–4 years, 23% 5–12 years, and 48% 13–17 years. Overall, 813 had a respiratory distress impression, and 82% (670/813) had a respiratory assessment. Compared to < 1 year, there was a twofold increase in the odds of respiratory assessment documentation among those 1–4 years (OR = 2.28, 95% CI = 1.48–3.54), a threefold increase for 5–12 years (OR = 3.02, 95% CI = 1.79–5.09), and a fivefold increase for 13–17 years (OR = 4.77, 95% CI = 2.29–9.94). Medication was administered to 788 patients, and 60% (469/788) had weight/length-based tape documented. This was similar among age categories (< 1 year = 67%, 1–4 years = 68%, 5–12 years = 63%, ≥ 13 years = 56%; p = .07). Finally, 36% (n = 3601) were not transported. Overall, 34% (n = 1214) had a BSVS documented. Compared to those < 1 year, there was a fourfold increase in the odds of BSVS documentation among those 1–4 years (OR = 4.10, 95% CI = 2.01–8.35), a 23-fold increase for those 5–12 years (OR = 22.80, 95% CI = 11.60–44.81), and an almost 38-fold increase among those ≥ 13 years (OR = 38.06, 95% CI = 19.51–74.26). Conclusion: These results can serve as a baseline of NESMQA performance, facilitating national and state-to-state comparisons. Strategies to improve performance on NEMSQA measures evaluated in this study should be investigated.
|