ABSTRACTS
Improving Prehospital Provider Confidence in Providing End-of-Life CareAuthor: Bianca Coleman, Kevin Collopy, and Margaret Spruill | | Associate Authors:
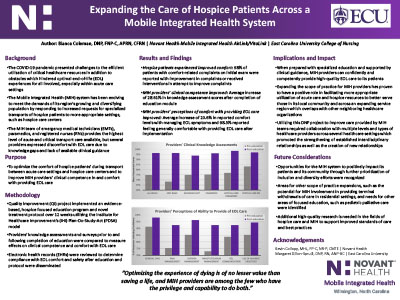
Introduction: Out-of-hospital patient care and transport of hospice patients are increasing, and traditional prehospital patient care protocols are not designed for optimal end-of-life (EOL) care. With the rise in frequency and complexity of care for patients nearing EOL, prehospital providers increasingly report feeling ill-equipped to meet such demands due to knowledge gaps and limited clinical guidance in their treatment protocols. Objective: To evaluate a clinical practice project aimed at expanding a Mobile Integrated Health (MIH) team's capabilities of competently and confidently providing evidence-based EOL care. Methods: The Novant Health New Hanover Regional Medical Center Institutional Review Board deemed this project a valid quality improvement (QI) initiative. A continuous QI process was performed using the Plan-Do-Study-Act (PDSA) model, which included developing evidence-based EOL-specific protocols and implementing them through a standardized education program. Participants completed pre- and postprogram knowledge assessments and surveys focused on their confidence levels in providing EOL care. Project leaders reviewed electronic health records (EHRs) to assess levels of compliance with EOL comfort and safety interventions, and data from provider testing and surveys were analyzed to determine the interventions' effects on clinical competence and comfort with providing EOL care. Results: One hundred and forty providers participated in the intervention, including EMTs (32.14%), Advanced EMTs (17.86%), paramedics (7.86%), critical care paramedics (21.43%), and critical care nurses (20.71%). After the education and protocol deployment, there was an increase in pre- to post-program knowledge assessment scores increased after education and protocol deployment, from 75.14% pretest to 96.64% post-test. Additionally, pre- to postsurvey responses revealed a 72.24% decrease in providers reporting a lack of confidence in managing EOL symptoms and a 78.69% decrease in providers reporting they were not comfortable providing general EOL care after implementation. One hundred and eighty-one patients were transported during the study period and included in the analysis. Most (98.3%) received documented interventions, indicating compliance with hospice-focused protocols. Conclusion: Prehospital provider knowledge and confidence in providing EOL improved and newly developed protocols were successfully utilized. These data suggest that prehospital providers can be trained to provide appropriate EOL care. Additional high-quality research is required in hospice care and MIH to support improved standards of care and best practices.
|