ABSTRACTS
A Statewide Evaluation of Potentially Undertriaged Trauma Patients in the Prehospital SettingAuthor: Daisy Banta, Jessica Rosner, Cam Crittenden, Remle P. Crowe, Brent J. Myers, Antonio R. Fernandez | | Associate Authors:
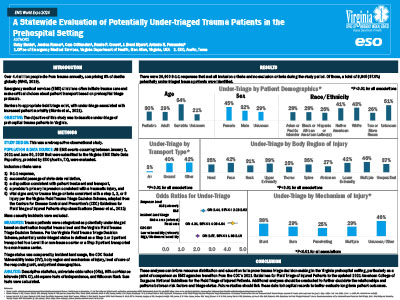
Introduction: Barriers to appropriate emergency medical service (EMS) triage of injured patients exist, with undertriage associated with increased mortality. Objective: To describe undertriage of Virginia prehospital trauma patients. Methods: This retrospective case-control study evaluated EMS incidents submitted to the Virginia Office of EMS from January 1, 2021, to June 30, 2023. Inclusion criteria were 9-1-1 response, patient treatment/transport disposition, primary impression indicating traumatic injury, and vital signs and/or trauma triage criteria consistent with any step in the Virginia Field Trauma Triage Decision Scheme. Mass casualty incidents were excluded. For this study, potentially undertriaged status was defined as a Step 1 or 2 patient transported to a Level III or nontrauma center or a Step 3 patient transported to a nontrauma center. Triage status was compared by incident characteristics, the CDC Social Vulnerability Index (SVI), body region, mechanism of injury, responding unit level, and patient demographics. Descriptive statistics, univariate odds ratios (ORs), 95% confidence intervals (95% CI), chi-square tests, and Wilcoxon rank sum tests were calculated. Results: In total, 26,600 incidents were evaluated. Of those, 9845 (37.0%) were potentially undertriaged. Odds of undertriage increased when the responding unit level was Basic Life Support compared to Advanced (OR = 2.44, 95% CI = 2.28–2.62). Patients transported by air were undertriaged significantly less often (2.8%) than patients transported by ground (39.5%). Higher proportions of undertriage occurred among patients with unknown/other mechanisms of injury (45.8%) compared to blunt (37.7%), burn (29.4%), multiple (28.5%), and penetrating (24.8%). Undertriage proportions were highest among patients with multiple body regions injured (45.9%), facial injuries (42.3%), and lower extremity injuries (42.0%). Higher proportions of undertriage occurred among geriatric patients (53.5%) compared to adult (29.2%) or pediatric (30.3%) and females (44.7%) compared to males (31.6%). Among racial groups, undertriage was higher among patients of unknown race (50.8%), followed by White (42.7%) and Native American (41.0%) patients. Odds of undertriage were increased in rural compared to metro areas (OR = 4.34, 95% CI = 4.06–4.64) and in localities with medium/high SVI scores compared to localities with the lowest score (OR = 2.07, 95% CI = 1.96–2.19). Conclusion: Nearly 40% of trauma patients were potentially undertriaged. These analyses can inform resource distribution and education to improve trauma triage decision-making. Future studies should link these data with hospital outcomes.
|