ABSTRACTS
Association Between EMS Agency Toolbox and Pain Management Practices by Race/EthnicityAuthor: Samuel Schow, BA, EMT-P, CHW | | Associate Authors:
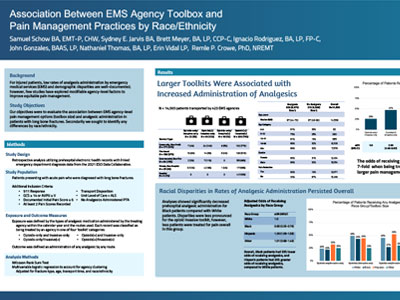
Background For injured patients, low rates of analgesia administration by emergency medical services (EMS) and demographic disparities are well documented; however, few studies have explored modifiable agency-level factors to improve equitable pain management. Our objectives were to evaluate the association between EMS agency-level pain management options and analgesia administration and identify any differences by race/ethnicity among patients with long bone fractures. Methods
We conducted a retrospective analysis using the 2021 ESO Data Collaborative. We included patients with hospital- Results We analyzed records for 14,560 patients transported by 423 agencies. All agencies carried opioids and delivered medications intravenously or intramuscularly. Additionally, most agencies had nonopioids and noninvasive routes available (79%, N = 336). Forty-nine (12%) agencies carried nonopioids but used only invasive routes, and 22 (5%) agencies only carried opioids and used invasive routes. There was a 7-fold increase in odds of analgesia for patients treated by agencies that carried nonopioids and noninvasive routes compared to agencies carrying only opioids and invasive routes (aOR: 7.37, 95% CI: 4.72-11.50). Nevertheless, Black patients had 35% lower odds of receiving analgesia compared to their White counterparts (aOR: 0.65, 95% CI: 0.55-0.76). Conclusion In this multi-agency cohort, patients were substantially more likely to receive analgesia if the transporting EMS agency had analgesic options beyond opioids by invasive routes; however, independent of agency analgesic options, Black patients remained less likely to receive analgesia. Limitations include possible misclassification of a medication carried for nonanalgesic indications.
|