ABSTRACTS
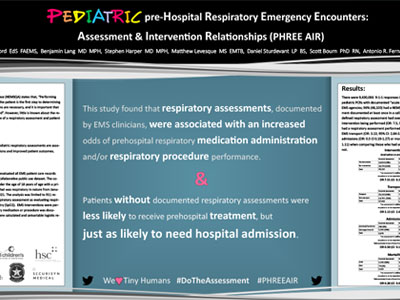
Pediatric preHospital Respiratory Emergency Encounters: Assessment and Intervention Relationships (PHREE AIR)Author: Stephanie Ashford, EdS, FAEMS | | Associate Authors:
Introduction The National EMS Quality Alliance (NEMSQA) states that, “Performing the respiratory assessment on the patient is the first step to determining if additional clinical interventions are necessary, and it is important that this process in care be measured.” However, little is known about the relationship with the performance of a respiratory assessment and patient outcomes. Objective To determine if documented pediatric respiratory assessments are associated with increased interventions and improved patient outcomes. Methods This retrospective cohort study evaluated all EMS patient care records (PCR) from the 2021 ESO Data Collaborative public use dataset. The cohort consisted of all patients under the age of 18 years of age with a primary or secondary impression that was respiratory in nature from January 1, 2021, to December 31, 2021. The analysis was limited to 9-1-1 responses. NEMSQA defines a respiratory assessment as evaluating respiratory rate (RR) and pulse oximetry (SpO2). EMS interventions were performed if at least one respiratory medication or procedure was documented. Descriptive statistics were calculated. Where appropriate, chi-squared tests, Fisher’s Exact tests, and univariable logistic regression were performed. Results
There were 8,296,774 9-1-1 responses in 2021. Of those, 50,004 were pediatric PCRs with documented “acute respiratory distress” from 1645 EMS agencies; 96% (48,100) had a NEMSQA-defined respiratory assessment documented at least once in a call. Patients with a NEMSQA-defined respiratory assessment had over 7 times higher odds of an EMS intervention being performed (OR: 7.5, 95% CI 6.34-8.90). Patients who had a respiratory assessment performed also had 3 times higher odds of EMS transport (OR: 3.13, 95% CI: 2.84-3.45). There was no difference in admissions (OR: 0.5 CI 0.19- Conclusion This study found that respiratory assessments, documented by EMS clinicians, were associated with an increased odds of prehospital respiratory medication administration and/or respiratory procedure performance. Patients without documented respiratory assessments were less likely to receive prehospital medication or intervention, but just as likely to need hospital admission. Further study should examine expanded respiratory assessment types and their intervention relationships.
|