ABSTRACTS
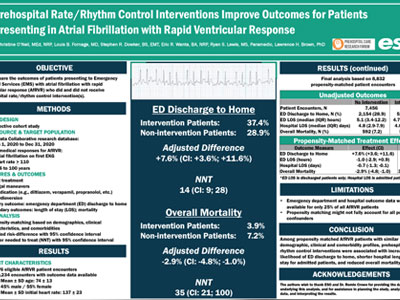
Prehospital Rate / Rhythm Control Interventions Improve Outcomes for Patients Presenting in Atrial Fibrillation with Rapid Ventricular ResponsAuthor: Christine O’Neil, MEd, NRP | | Associate Authors:
Introduction
There is little evidence regarding prehospital rate and rhythm control interventions for patients with atrial fibrillation who present with rapid ventricular response (AfRVR). The purpose of this study was to compare emergency department (ED) Methods
This retrospective cohort study used the calendar year 2021 ESO Research Collaborative (Austin, TX) dataset to identify 9- Results There were 10,234 eligible patients presenting with AfRVR who had ED and hospital outcome data available; after propensity matching, 8832 patients were retained in the analysis: 1376 (15.6%) with prehospital intervention, and 7456 (84.4%) similar patients without intervention. ED discharge to home occurred for 37.4% of the intervention patients vs 28.9% of the nonintervention patients (adjusted difference: +7.6%, CI: +3.6%; +11.6%; NNT: 14, CI: 9; 28). Among admitted patients, median (IQR) LOS was 4 (2-7) days for intervention patients vs 5 (3-8) days for nonintervention patients (adjusted difference: –0.7 days, CI: –1.3; –0.1). Mortality among intervention patients was 3.9% vs 7.2% for nonintervention patients (adjusted difference: –2.9%, CI: –4.8%; –1.0%; NNT: 35, CI: 21-100). Conclusion Among propensity score matched AfRVR patients with similar demographic, clinical and comorbidity profiles, prehospital rate or rhythm control interventions were associated with increased likelihood of ED discharge to home (NNT = 14); shorter hospital length of stay for admitted patients (~ 1 day); and reduced overall mortality (NNT = 35).
|