ABSTRACTS
Determining Appropriate EMS Transport Decisions to a Free-Standing Emergency Department Using the Rapid Emergency Medicine ScoreAuthor: Douglas Randell | | Associate Authors: Jordan Strange | Remle P. Crowe
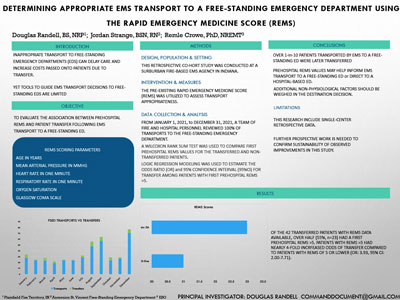
Background/Objective Inappropriate transport to free-standing Emergency Departments (EDs) can delay care and increase costs passed onto patients due to transfer, yet tools to guide EMS transport decisions to free-standing EDs are limited. The Rapid Emergency Medicine Score (REMS) is a simple risk-stratification tool that uses variables readily collected in the prehospital setting. Our objective was to evaluate the association between prehospital REMS and patient transfer following EMS transport to a free-standing ED. Methods In this retrospective cohort study, we analyzed EMS records from a Midwestern fire-based service and outcome data from a free-standing ED. We identified all adult EMS transports to the free-standing ED from January 1, 2021 to December 31, 2021. Our primary outcome was patient transfer. Based on patient age, mean arterial pressure, pulse rate, respiratory rate, oxygen saturation, and Glasgow Coma Scale, REMS values range from 0-26 with scores > 5 predicting patient admission. A Wilcoxon Rank Sum test was used to compare first prehospital REMS values for transferred and nontransferred patients. Logistic regression modeling was used to estimate the odds ratio (OR) and 95% confidence interval (95% CI) for transfer among patients with first prehospital REMS > 5. Results We analyzed 379 EMS transports to the free-standing ED. Overall, 12% (N = 47) were subsequently transferred to a hospital-based ED. Prehospital data to calculate REMS was available for 297 (78%). First prehospital REMS was significantly higher among transferred patients (median: 6, IQR: 3-7) compared to nontransferred patients (median: 3, IQR: 2-5, P < 0.01). Of the 42 transferred patients with REMS data available, over half (55%, N = 23) had a first prehospital REMS > 5. Patients with REMS > 5 had nearly 4-fold increased odds of transfer compared to patients with REMS of 5 or lower (OR: 3.93, 95% CI: 2.00-7.71). Transfer reasons for patients with REMS of 5 or less (N = 19) included behavior-related concerns, surgery, or other services the free-standing ED could not provide. Conclusion Over 1 in 10 patients transported by EMS to a free-standing ED were later transferred. Prehospital REMS values may help inform EMS transport to a free-standing ED or direct to a hospital-based ED. Additional nonphysiological factors should be weighed in the destination decision. Limitations include single-center retrospective data.
|